P - (386) 672-1023 | F - (386) 263-2996
P - (386) 672-1023 | F - (386) 263-2996


Heart Arrhythmia Treatments
in Daytona Beach, FL
Fluttering, palpitations, or a light feeling in your chest can all be potential signs you are suffering from an arrhythmia. From atrial fibrillation(afib), premature beats (PVCs), or ventricular tachycardia we can help.
No one plans on having heart problems, but if you do you need to find a doctor you can trust. At Complete Cardiology Care we staff Cardiologists and Electrophysiologists that treat patients with arrhythmias in Daytona Beach, Ormond Beach, Palm Coast, Deltona, Deland, and the surrounding areas.
4 Million
Suffer from recurrent
arrhythmias in the U.S.
Atrial fibrillation
Most common arrhythmia diagnosed
65-70
Mean age of Afib diagnosis.
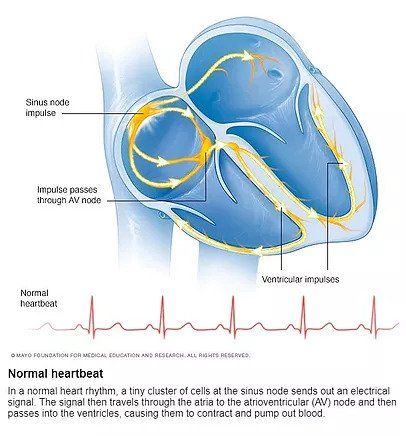
A Normal Heart Beat
What is a heart arrythmia?
Heart rhythm problems (heart arrhythmias) occur when the electrical impulses that coordinate your heartbeats don't work properly, causing your heart to beat too fast, too slow or irregularly.
Heart arrhythmias may feel like a fluttering or racing heart and may be harmless. However, some heart arrhythmias may cause bothersome — sometimes even life-threatening — signs and symptoms.
Heart arrhythmia treatment can often control or eliminate fast, slow or irregular heartbeats. In addition, because troublesome heart arrhythmias are often made worse — or are even caused — by a weak or damaged heart, you may be able to reduce your arrhythmia risk by adopting a heart-healthy lifestyle.
-
What are some types of heart arrhythmias?
Doctors classify arrhythmias not only by where they originate (atria or ventricles) but also by the speed of heart rate they cause:
- Tachycardia. This refers to a fast heartbeat — a resting heart rate greater than 100 beats a minute.
- Bradycardia. This refers to a slow heartbeat — a resting heart rate less than 60 beats a minute
Not all tachycardias or bradycardias mean you have heart disease. For example, during exercise it's normal to develop a fast heartbeat as the heart speeds up to provide your tissues with more oxygen-rich blood. During sleep or times of deep relaxation, it's not unusual for the heartbeat to be slower.
-
Tachycardias in the atria
Tachycardias originating in the atria include:
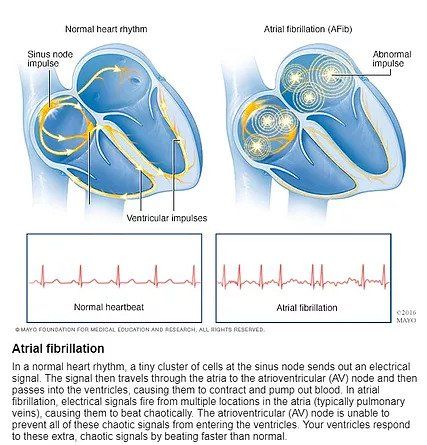
- Atrial fibrillation. Atrial fibrillation is a rapid heart rate caused by chaotic electrical impulses in the atria. These signals result in rapid, uncoordinated, weak contractions of the atria. The chaotic electrical signals bombard the AV node, usually resulting in an irregular, rapid rhythm of the ventricles. Atrial fibrillation may be temporary, but some episodes won't end unless treated. Atrial fibrillation may lead to serious complications such as stroke.
- Atrial flutter. Atrial flutter is similar to atrial fibrillation. The heartbeats in atrial flutter are more-organized and more-rhythmic electrical impulses than in atrial fibrillation. Atrial flutter may also lead to serious complications such as stroke.
- Supraventricular tachycardia. Supraventricular tachycardia is a broad term that includes many forms of arrhythmia originating above the ventricles (supraventricular) in the atria or AV node.
- Wolff-Parkinson-White syndrome. In Wolff-Parkinson-White syndrome, a type of supraventricular tachycardia, there is an extra electrical pathway between the atria and the ventricles, which is present at birth. However, you may not experience symptoms until you're an adult. This pathway may allow electrical signals to pass between the atria and the ventricles without passing through the AV node, leading to short circuits and rapid heartbeats.
-
Tachycardias in the ventricles
Tachycardias occurring in the ventricles include:
- Ventricular tachycardia. Ventricular tachycardia is a rapid, regular heart rate that originates with abnormal electrical signals in the ventricles. The rapid heart rate doesn't allow the ventricles to fill and contract efficiently to pump enough blood to the body. Ventricular tachycardia can often be a medical emergency. Without prompt medical treatment, ventricular tachycardia may worsen into ventricular fibrillation.
- Ventricular fibrillation. Ventricular fibrillation occurs when rapid, chaotic electrical impulses cause the ventricles to quiver ineffectively instead of pumping necessary blood to the body. This serious problem is fatal if the heart isn't restored to a normal rhythm within minutes. Most people who experience ventricular fibrillation have an underlying heart disease or have experienced serious trauma, such as being struck by lightning.
- Long QT syndrome. Long QT syndrome is a heart disorder that carries an increased risk of fast, chaotic heartbeats. The rapid heartbeats, caused by changes in the electrical system of your heart, may lead to fainting, and can be life-threatening. In some cases, your heart's rhythm may be so erratic that it can cause sudden death. You can be born with a genetic mutation that puts you at risk of long QT syndrome. In addition, several medications may cause long QT syndrome. Some medical conditions, such as congenital heart defects, may also cause long QT syndrome.
-
Bradycardia - A slow heart beat
Although a heart rate below 60 beats a minute while at rest is considered bradycardia, a low resting heart rate doesn't always signal a problem. If you're physically fit, you may have an efficient heart capable of pumping an adequate supply of blood with fewer than 60 beats a minute at rest.
In addition, certain medications used to treat other conditions, such as high blood pressure, may lower your heart rate. However, if you have a slow heart rate and your heart isn't pumping enough blood, you may have one of several bradycardias, including:
- Sick sinus syndrome. If your sinus node, which is responsible for setting the pace of your heart, isn't sending impulses properly, your heart rate may be too slow (bradycardia), or it may speed up (tachycardia) and slow down intermittently. Sick sinus syndrome can also be caused by scarring near the sinus node that's slowing, disrupting or blocking the travel of impulses.
- Conduction block. A block of your heart's electrical pathways can occur in or near the AV node, which lies on the pathway between your atria and your ventricles. A block can also occur along other pathways to each ventricle. Depending on the location and type of block, the impulses between the upper and lower halves of your heart may be slowed or blocked. If the signal is completely blocked, certain cells in the AV node or ventricles can make a steady, although usually slower, heartbeat. Some blocks may cause no signs or symptoms, and others may cause skipped beats or bradycardia.
-
Diagnosis of arrhythmias in Daytona Beach, FL
To diagnose a heart arrhythmia, your doctor will review your symptoms and your medical history and conduct a physical examination. Your doctor may ask about — or test for — conditions that may trigger your arrhythmia, such as heart disease or a problem with your thyroid gland. Your doctor may also perform heart-monitoring tests specific to arrhythmias. These may include:
- Electrocardiogram (ECG). During an ECG, sensors (electrodes) that can detect the electrical activity of your heart are attached to your chest and sometimes to your limbs. An ECG measures the timing and duration of each electrical phase in your heartbeat.
- Holter monitor. This portable ECG device can be worn for a day or more to record your heart's activity as you go about your routine.
- Event recorder or Mobile Cardiac Telemetry. For sporadic arrhythmias, you keep this portable ECG device available, attaching it to your body and pressing a button when you have symptoms. This lets your doctor check your heart rhythm at the time of your symptoms.
- Echocardiogram. In this noninvasive test, a hand-held device (transducer) placed on your chest uses sound waves to produce images of your heart's size, structure and motion.
- Implantable loop recorder. If your symptoms are very infrequent, an event recorder may be implanted under your skin in the chest area to continually record your heart's electrical activity and detect abnormal heart rhythms.
If your doctor doesn't find an arrhythmia during those tests, he or she may try to trigger your arrhythmia with other tests, which may include:
- Stress test. Some arrhythmias are triggered or worsened by exercise. During a stress test, you'll be asked to exercise on a treadmill or stationary bicycle while your heart activity is monitored. If doctors are evaluating you to determine if coronary artery disease may be causing the arrhythmia, and you have difficulty exercising, then your doctor may use a drug to stimulate your heart in a way that's similar to exercise.
- Tilt table test. Your doctor may recommend this test if you've had fainting spells. Your heart rate and blood pressure are monitored as you lie flat on a table. The table is then tilted as if you were standing up. Your doctor observes how your heart and the nervous system that controls it respond to the change in angle.
- Electrophysiological testing and mapping. In this test, doctors thread thin, flexible tubes (catheters) tipped with electrodes through your blood vessels to a variety of spots within your heart. Once in place, the electrodes can map the spread of electrical impulses through your heart.
In addition, your cardiologist can use the electrodes to stimulate your heart to beat at rates that may trigger — or halt — an arrhythmia. This allows your doctor to see the location of the arrhythmia, what may be causing it and what treatments may help. Your doctor may also use this test to assess the likelihood that you will develop an arrhythmia if you have certain conditions that increase your risk.
-
Treatment of arrhythmias in Daytona Beach, FL
If you have an arrhythmia, treatment may or may not be necessary. Usually, it's required only if the arrhythmia is causing significant symptoms or if it's putting you at risk of a more serious arrhythmia or arrhythmia complication.
Treating slow heartbeats
If slow heartbeats (bradycardias) don't have a cause that can be corrected, doctors often treat them with a pacemaker because there aren't any medications that can reliably speed up the heart.
A pacemaker is a small device that's usually implanted near your collarbone. One or more electrode-tipped wires run from the pacemaker through your blood vessels to your inner heart. If your heart rate is too slow or if it stops, the pacemaker sends out electrical impulses that stimulate your heart to beat at a steady rate.
Treating fast heartbeats
For fast heartbeats (tachycardias), treatments may include one or more of the following:
- Vagal maneuvers. You may be able to stop an arrhythmia that begins above the lower half of your heart (supraventricular tachycardia) by using particular maneuvers that include holding your breath and straining, dunking your face in ice water, or coughing. These maneuvers affect the nervous system that controls your heartbeat (vagus nerves), often causing your heart rate to slow. However, vagal maneuvers don't work for all types of arrhythmias.
- Medications. For many types of tachycardia, you may be prescribed medication to control your heart rate or restore a normal heart rhythm. It's very important to take any anti-arrhythmic medication exactly as directed by your doctor in order to minimize complications. If you have atrial fibrillation, your doctor may prescribe blood-thinning medications to help keep dangerous blood clots from forming.
- Cardioversion. If you have a certain type of arrhythmia, such as atrial fibrillation, your doctor may use cardioversion, which can be conducted as a procedure or by using medications. In the procedure, a shock is delivered to your heart through paddles or patches on your chest. The current affects the electrical impulses in your heart and can restore a normal rhythm.
- Catheter ablation. In this procedure, your doctor threads one or more catheters through your blood vessels to your heart. Electrodes at the catheter tips can use heat, extreme cold or radiofrequency energy to damage (ablate) a small spot of heart tissue and create an electrical block along the pathway that's causing your arrhythmia.
Implantable devices
Treatment for heart arrhythmias also may involve use of an implantable device:
- Pacemaker. A pacemaker is an implantable device that helps control abnormal heart rhythms. A small device is placed under the skin near the collarbone in a minor surgical procedure. An insulated wire extends from the device to the heart, where it's permanently anchored. If a pacemaker detects a heart rate that's abnormal, it emits electrical impulses that stimulate your heart to beat at a normal rate.
- Implantable cardioverter-defibrillator (ICD). Your doctor may recommend this device if you're at high risk of developing a dangerously fast or irregular heartbeat in the lower half of your heart (ventricular tachycardia or ventricular fibrillation). If you have had sudden cardiac arrest or have certain heart conditions that increase your risk of sudden cardiac arrest, your doctor may also recommend an ICD. An ICD is a battery-powered unit that's implanted under the skin near the collarbone — similar to a pacemaker. One or more electrode-tipped wires from the ICD run through veins to the heart. The ICD continuously monitors your heart rhythm. If it detects an abnormal heart rhythm, it sends out low- or high-energy shocks to reset the heart to a normal rhythm. An ICD doesn't prevent an abnormal heart rhythm from occurring, but it treats it if it occurs.
Don't let your arrhythmia control your life and get treated today
If you are curious how we can help you with your arrhythmia symptoms, please reach out to us. We are currently accepting new patients. Complete Cardiology Care staffs Cardiologists and Electrophysiologist that serve patients in Ormond Beach, Daytona Beach, New Smyrna Beach, Port Orange, Deltona, Deland, and the surround areas.
Our Cardiologists and Electrophysiologists take nearly all insurances. We accept Aetna, AARP Medicare Complete, Blue Cross / Blue Shield, Cigna, Florida Healthcare, Florida Hospital Care Advantage, Freedom Health, Health First Health, Humana PPO - out of network benefits apply, Medicare, Optimum Healthcare, Railroad Medicare, Tricare, United Healthcare, VHN, Wellcare.
We are also a partner with the VA and are proud to serve those who have served our country!
Self Pay Cardiology services are available too! Call and ask for our price list.
LOCATION
Ormond Beach
1240 W Granada Blvd
2nd Floor
Ormond Beach, FL 32174
CLINIC HOURS - Ormond
- Monday
- -
- Tuesday
- -
- Wednesday
- -
- Thursday
- -
- Friday
- -
- Saturday
- Closed
- Sunday
- Closed
All statements on this website are no substitution for actual medical advice. They are merely informational content and personal treatment without the guidance of a licensed practitioner is never recommended. Complete Cardiology Care assumes no responsibility for actions taken.

